With an aging population, the rise of chronic diseases and the need to develop a healthcare infrastructure in emerging countries, there is a strong need to transform the care that we receive today.
Authors:
Adi Shieber, Yan Vainter, Freescale Semiconductor
Moving from a treatment based system to a prevention approach.
In our current healthcare system the patient is not asked to take an active role. Most of us have no knowledge about the human body or about the early signs of a disease. Take for example, you can ask people about the balance of their bank account but most of them will not be able to tell you what their blood pressure or heart rate is. The outcome is that people usually react too late and when they finally go to their doctor and have a diagnosis and potentially the prescribed treatment is more expensive and has more physiological impact than if the disease had been detected earlier.
The first step toward a prevention based system is to educate people about their own
health and to provide them with the tools which allow them to take ownership of their health such as measurement devices to simply assess their vital signs and thus detect the early signs of a disease or use treatment devices like auto-injectors to self-administrate their drugs. To make this possible, medical device manufacturers need to bring professional equipment into peoples’ houses and this brings with it several challenges. Such devices would have to be cost effective to make them accessible to the broadest audience possible plus these devices will also have to be portable which dictates that they are battery operated and naturally they will have to communicate via wireless.
These devices must also be easy to use as the target audience will no longer be the professionals so development of advanced user interfaces, safety, security and high levels of automated operation will be the key to success.
New technology for cost effective, portable and connected medical devices
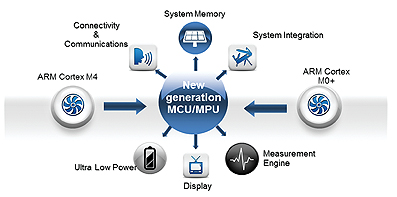
Those new requirements for medical device designers, cost effective, easy to use, portable and wireless connectivity were until recently unattainable goals due to many technological challenges, but recent advances from semiconductors suppliers like Freescale using ARM® low power processors to design advanced Kinetis® MCUs that use Cortex™-M4 and M0+ processor cores are making this a reality today. The performances that these systems can deliver make the requirements discussed above achievable.
A perfect example is the blood glucose monitor. This device usually has 5 or 6 different modes of operation: standby while in your pocket/bag, wake-up and wait for a blood drop to be applied on the test strip, measurement of the electrochemical reaction, processing of the samples, logging of the results, display of the data.
To run all of these steps older processor technology would have to be working at its maximum performance operating point for the entire measurement cycle, except when in standby, which would be a massive drain on a battery and therefore would not have met the requirements for a portable device. Today however with the latest microcontroller devices that integrates that processing system on a single chip resulting in low power systems can more than half the energy used by the device and therefore can double the period of time between battery replacements or recharge cycles.
Helping to ensure a high level of safety and making the certification process easier are also key advantages of an integrated solution as the number of components in the system is reduced and the interaction between the different features are clearly documented.
One of the one the biggest concerns for medical device companies is the product certification process and to ensure that a component selected, used and certified in a product does not cease to be manufactured during the product lifetime. Freescale offers a formal 15 year longevity program to its medical customers, preventing an expensive re-certification of the product if a component goes out of production by a supplier. For Terms and Conditions and to obtain a list of available products please see: www.Freescale.com/productlongevity.
Case Study
A current and impressive example of what this advanced technology is enabling is the

Omnipod® from Insulet, a revolutionary tubeless insulin pump. Conventional pump therapy includes an insulin pump, reservoir, an infusion set and tubing that connect the insulin pump to the infusion set—keeping the patient tethered to the pump 24/7. The revolutionary OmniPod® design has only two parts: a wearable pod that delivers the insulin and a PDA-type device called a Personal Diabetes Manager (PDM).
The pod is worn for three days and then replaced with another pod. It holds 200 units of rapid-acting insulin, which covers the requirements of almost 95% of Type 1 diabetes patients.
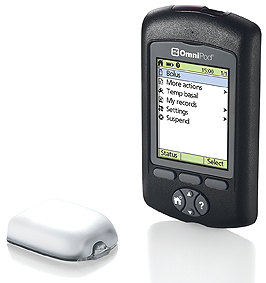
When it came time to find a silicon provider for their design, Insulet searched for a partner who could do a custom chip. Insulet saw that Freescale had the right microcontrollers to control size and cost for the disposable pods, and RF connectivity for the PDM and pod to communicate wirelessly.
Freescale worked with Insulet to design a custom ASIC through a close collaboration. The customized microcontroller design consumes very little power and enables communication between the PDM and the pod using an integrated 13.56 MHz radio. Through this technology alliance, a product was developed that meets the cost and reimbursement structure for the marketplace, in a small, wireless full-featured device.
The next phase in utilising technology to reduce healthcare costs is to move from a hospital/doctor centric system to a decentralized approach in which people measure their vital signs by themselves.
To address this issue we must first get all these medical devices, both measurement and treatment, connected so the information can reach the doctor through secured databases without the need for the patient to be physically present.
Smart connected homes are the basis of this future decentralized system where patients can transmit vital health data from their home to the physician’s office and in turn receive personalized health coaching tips from the practitioner or smart knowledge based information systems based in server hubs that are collectively referred to as ‘the cloud.’ Furthermore, in smart connected homes networked devices and Telehealth systems can act in pre-programmed ways if a medical problem were to occur within the home of a patient, for example a family member or the care centre, depending pre-set automatic alert levels will automatically be alerted should the situation warrant it. Home Telehealth systems are expected to become ubiquitous in smart connected homes and will generally consist of a central health hub managing multiple biometrics devices as well as security and assisted living sensors. This will allow people with illnesses or disabilities to live within the comfort of their homes while retaining a high quality of life. There is compelling evidence to support the value of remote monitoring for individuals with chronic conditions, including:
• 35-56% reduction in mortality
• 47% reduction in risk of hospitalization
• 6 days reduction in length of hospital admission
• 65% reduction in office visits
• 40-64% reduction in physician time for checks and
• 63% reduction in transport costs
(Cleland et al 2005; Lee R, Goldberg et al, 2003; Scalvini S et al., 2001; Elsner et al, 2006; Van Ginneken et al 2006)
The next phase in introducing Telehealth is effective delivery of a careplan to patients suffering from chronic disease, home Telehealth devices should focus on users and services and make the underlying electronic technology used in patient centred devices as unobtrusive as possible. Patients have to be comfortable and confident that they can trust the devices delivering their healthcare. The platform technologies should be flexible enough to accommodate for device personalization based on diagnosis and patient-led requirements and have a user interface that is simple and understandable. The technology described above allows device manufacturers to develop such user interfaces and make their final products as user friendly as possible using a reference platform. For connectivity the platform features ethernet and WiFi™ to ease internet connectivity to the cloud and USB, Bluetooth® and ZigBee® to guarantee interoperability with biometric device connectivity that is compliant to the Continua alliance guidelines.
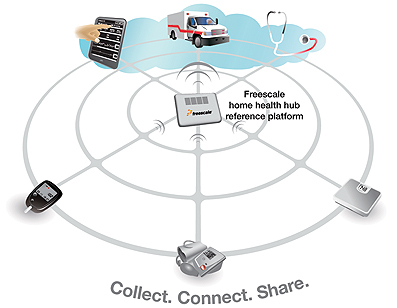
Advanced security features are also provided by the reference platform like authenticated startup, and hardware-based encryption that will allow designers to implement data privacy schemes and governed levels of medical data access. These embedded security features will also allow for simplified integration of Telehealth platforms into medical health networks. For example the Home Health Hub Reference Platform is being pre-integrated with Microsoft’s Healthvault cloud service where authenticated and encrypted home based medical measurement results can be transmitted and then monitored by a triage centre that would be alerted in real-time if a vital statistic moves outside previously set limits.
Future areas for improvements that can help deliver an efficient and cost effective healthcare is the diagnosis of the patient’s illness. Today this process has already changed in some hospitals where nurses can use instruments to perform diagnostic analysis at the bed side saving time, money and making the patient’s life more comfortable. The next step will be to deploy those devices at local clinics and the finally in people’s homes so they can do a self-screening. The first of its kind in homes has been around for years: pregnancy tests. The second is changing the life of millions of diabetics: the blood glucose monitor. What’s coming next? The Freescale medical team driven by Dr.Fernandez (neurosurgeon and EE) is working on a new generation of biochemical sensors. This technology is based on Ion Sensitive Field Effect Transistors (IsFETs) and these sensors are then used to create Immunological sensitive FETs ImFETs, which can be used to detect not only pH, but also to detect antigens and antibodies of specific pathogens that cause a wide array of infectious diseases.
Future Possibilities
Wearable devices like smart plasters to collect body temperature, respiration, ECG, are getting really close but their size, weight, power consumption and price still need to be lowered to bring more comfort to the patients at an acceptable price. The latest advances with highly integrated system on a chip microcontroller and many types of connectivity are moving medical electronics forward at a rapid pace. Another exciting innovation is in energy harvesting from the heat of the body or from movement to deliver the power needed to run these portable healthcare devices continuously without any need for bulky batteries and this will move the size and weight of such products into unobtrusive, wearable accessories.
The industry we anticipate will be able to deliver such solutions in the next 5 years.
www.freescale.com


