The Impact That Wearables and the IoT Will Have on Patient Care
Reducing the risk of medical complications in patients with chronic conditions has long posed a formidable challenge for healthcare providers. Now, however, breakthroughs in wearable technology – enabled largely by the phenomenon of the Internet of Things (IoT) – are poised to help dramatically reduce the chances of acute complications.
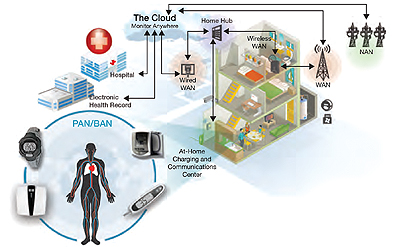
The IoT reduces the risk of complications by making it possible to easily, accurately and continuously gather and share information about patient health, using portable medical devices within a network of microcontrollers and applications processors that connects with the cloud and other networks.
These connected devices can automatically track vital signs and patient activities, detect changes that could indicate potential problems and provide alerts to caregivers – ensuring a timely response and a better chance of averting problems.
Author: Dr. Jose Fernandez Villasenor, MD, EE, Healthcare Marketing Manager at Freescale Semiconductor
Introduction
Patients suffering from chronic conditions rely on accurate treatment control and need biometric parameters to be tracked 24/7. Portable medical devices that are connected through service providers to hospitals will enable physicians to better assure that patient parameters and treatments are followed and controlled at home by detecting changes in the data collected through the edge/sensing framework.

Once a patient is diagnosed with a chronic degenerative disease, the odds of having an acute complication are directly tied to how well the treatment can be controlled. A chronic degenerative disease is as its name explains, chronic, because there is no cure for it. The patient will have the condition for life, and it is important to note that chronic conditions are ultimately degenerative because they tend to worsen over time.
Additionally, because no cure exists for chronic disease, the human body will make certain adaptations to lifelong pharmacological treatment and effects like tachyphylaxis can appear. Tachyphylaxis is a cultivated tolerance to drugs in which the body grows accustomed to a repeatedly used drug and more dosage is required every time—until eventually there could be no response to a drug at all.
Sometimes a double or triple pharmacological treatment will be needed just to have the same healthy effect that one drug had in the past. Therefore, reliably monitoring how well the drug is helping the patient is critical. However, doctors cannot expect to see patients two or three times a day just to measure test results or review patient vital signs. Usually one doctor visit every month is considered a good case.
Finally, the aging of the body also plays a part since normal aging diminishes the functionality of human organs over time. As one can expect, the conditions of the patient will not improve with time, and a lack of disciplined adherence to treatment could speed complications.
The IoT for Healthcare
As we enter a new era of computing technology called the Internet of Things (IoT), smart machines are interacting and communicating with other machines, objects, environments and infrastructures, resulting in volumes of generated data and the processing of that data into useful actions, making life much easier for human beings. The IoT will be the key to enabling better preventative healthcare and disease-control solutions for people, through edge/sensing nodes that consist of sensors, microcontrollers, microprocessors, and connectivity and energy sources connecting to IoT gateways (which in turn connect to the cloud and data centers) through service providers.
Medical devices can track patient vital signs and treatment adhesion automatically. For example, medical patches and sport watches can gather information from patients. Measuring the data and not sending it to the proper people just wastes money and time; however, if certain parameters go above or beyond the normal thresholds, notification through intelligent gateways should detect if the information is something worth transmitting or just storing for further report.
Some values could be life threatening, some could be important to forward to healthcare providers immediately and others could show how beneficial the drug is to the patient.
The Edge/Sensing Node
Most IoT edge nodes consist of sensors and maybe actuators, an embedded processor (typically an MCU), a connectivity engine and an energy source. Analog Front Ends (AFEs) are the primary interface between the patient and processing units. In order to relieve the patient of the burden of understanding what, when and how to take measurements, wearable devices address these issues automatically. Many of these devices are in the form of rings, watches, patches and other form factors that require zero user configuration therefore battery life and low-power performance are an essential part of the design.1
The following parameters need to be measured for the most common chronic degenerative diseases:
For patients with primary and secondary hypertension:

1. Blood pressure: systolic, diastolic, mean arterial pressure and heart rate. Current sensors need a cuff piece, making it impractical to monitor in a continuous mode. The oscillometric measurement mode that is used is prone to errors related to the movement of the patient. New technologies are being studied for small, cuff-less sensors like the wearable photoplethysmography (PPG) with a height sensor.2
For patients with Type 1 and Type 2 diabetes and gestational diabetes:

2. Blood glucose: could be measured depending on the adherence of the patient to the treatment, how well controlled the condition is, or specific needs for pharmacological treatment, current evaluation or continuous/regular adjustments just few times a day. Technologies for continuous blood glucose monitoring are available at the market.
For patients with cardiovascular pathologies:

3. Electrocardiography: Most commonly done through a 1 lead EKG requiring two main electrodes to make the differential of the lead and a reference electrode. It is often also used to feedback the noise and cancel potential noisy signals. Wearable EKG patches, enabled by Freescale, exist in the market today. This patch acquires the signal by integrating the electrodes in the device and with a wireless radio antenna. Some other devices like ring-type heart rate sensors are also being developed.
For patients suffering from any type of pulmonary obstructive disease like Chronic Obstructive Pulmonary Disease (COPD), asthma, pulmonary cancer or certain hematological diseases:

4. Pulse Oximetry: A pair of diodes is used to obtain the partial oxygen saturation levels, through logarithmic formulas, that also allow a PPG to be obtained.
Microcontrollers and Microprocessors
Once we have gathered the data from the sensors to conduct some basic algorithms, threshold detection and simple data analysis, we need to manage the data. It involves measuring and transmitting with high accuracy and in a prompt manner so that the manager can forward the information to the corresponding healthcare service provider.
Low-power performance is a requirement since all of these devices are usually battery operated. Encryption is also needed since the originating device transmits information and the patient’s data needs a minimum grade of security while being transmitted, especially in the wireless media.
Freescale’s Kinetis family microcontrollers (MCUs) are based on the ARM Cortex-M4 or ARM Cortex-M0. ARM microcontrollers have shown better power performance and memory capability compared to other MCUs architectures and have existing market enablement.3
For applications which require a reduction in the external analog components and integration with a powerful measurement engine, we recommend Freescale Kinetis K series MCUs with the following features:
• ARM Cortex-M4 (DSP/FPU)
• Precision mixed-signal, FlexMemory technology (EEPROM), HMI, connectivity and security
• 50–150MHz, 32KB–1MB, 32–256 pin
Specifically, the Kinetis K50 MCU integrates an analog measurement engine consisting of integrated operational and transimpedance amplifiers and high-resolution ADC and DAC modules.
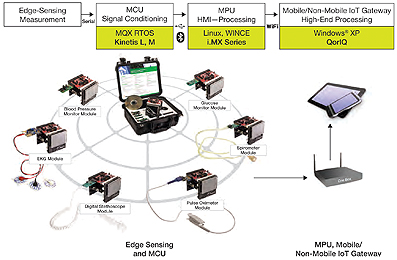
The family also features IEEE® 1588 Ethernet and hardware encryption, full-speed USB 2.0 On-The-Go with device charger detect capability and a flexible low-power segment LCD controller with support for up to 320 segments. The K50 measurement MCUs are also energy-efficient product solutions.
If power performance is required, then the Kinetis L series MCUs are recommended. Kinetis L series MCUs combine energy efficiency and ease of use of the ARM Cortex-M0+ processor with the performance, peripheral sets, enablement and scalability of the Kinetis 32-bit MCU portfolio.
Kinetis L series MCUs improve 8- and 16-bit MCU performance limitations by combining excellent dynamic and stop currents with superior processing performance, a broad selection of on-chip Flash memory densities and extensive analog, connectivity and HMI peripheral options.
Kinetis L series MCUs are also hardware and software compatible with the ARM Cortex-M4- based Kinetis K series, providing a scalable migration path to more performance, memory and feature integration.
IoT Gateway with Microcontrollers
IoT gateways will offload a lot of data center functionalities and will provision the services locally at the premise, and not only do if-this-then-that type of decision making for the edge/ sensing nodes hanging off of them, but also perform local big data analytics and only pass along the data to the cloud if needed. The IoT gateways can also send out meta data.
They will have lots of memory, and depending on if real-time capabilities are needed, would need RTOSs or standard operating systems.
Microprocessors like the i.MX 6 series from Freescale provide an excellent solution for the gateway that needs to drive an HMI touchscreen display, run the OS and the networking protocols like IPv6, 3G, Wi-Fi® and other wireless communication protocols and provide extensive computing performance.
i.MX 6 series of applications processors is the industry’s first truly scalable multicore platform that includes single-, dual- and quad-core families based on the ARM Cortex-A9 architecture. Pin-compatibility among four of the families means one platform investment by the customer can be leveraged and re-used across multiple product lines, thus reducing resource requirements and shortening time to market. The i.MX 6SoloLite is in a smaller package so it is not pin-to-pin compatible with the other families; however, there is software compatibility.
Connecting Mobile/Nonmobile Devices with Networking
The complete picture will not be ready without the last part—getting the data to the healthcare providers so that the decision for healthcare management or even preventing an acute complication of a chronic degenerative disease is detected early enough to be avoided.
We need processors that meet throughput requirements with robust real-time, point-to-point communication like QorIQ processors from Freescale.
We could have a potential scenario in which the gateway is indeed a mobile phone that controls and manages a series of edge/sensing devices. But, consider the case of an elderly patient who wants to live independently. A telehealth gateway that is easy to use and simple enough for them to set them up in their home is ideal.
Two series, based on Power Architecture, are recommended from Freescale. The QorIQ AMP series (T1–T5), based in the e6500 multithreaded 64-bit core at frequencies up to 2.5 GHz, includes the AltiVec vector processing unit that addresses high-bandwidth data processing and algorithmic-intensive computations.
The QorIQ P series multicore is pin and software compatible between the P1 and P2 families with single- and dual-core options. Low power and low cost with frequency ranges starting at 533 MHz to a dual core at 1.2 GHz, the P3 and P4 families are built on the e500mc core and feature four to eight cores running up to 1.5 GHz. Embedded Linux®, QNX® and INTEGRITY are some of the supported OSs.
Long-Term Benefits
The IoT will enable the patient to take control and be more active in his own treatment and recovery. It will lower the social and economic costs of overwhelmed physicians and nurses at hospitals and move roles and activities that were previously only performed at hospitals to patient homes, preventing acute complications and helping improve treatments for patients.
www.freescale.com
References
1. Wearable Medical Devices for Tele-Home Healthcare, K.Hung, Y.T. Zhang and B. Tai. Joint Research Center for Biomedical Engineering.
2. Wearable, cuff-less PPG-based blood pressure monitor with novel height sensor. Phillip A. Shaltis, Andrew Reisner, and H. Harry Asada; Proceedings of the 28th IEEE, EMBS Annual International Conference, New York City, U.S., August 30–September 3, 2006.
3. A Front-end Platform of the Network-based Intelligent Home Healthcare Embedded System. Shuo Tang, Weng Chi Chan, et al. 26th Annual International Conference IEEE EMBS.


